Thyroid Surgery
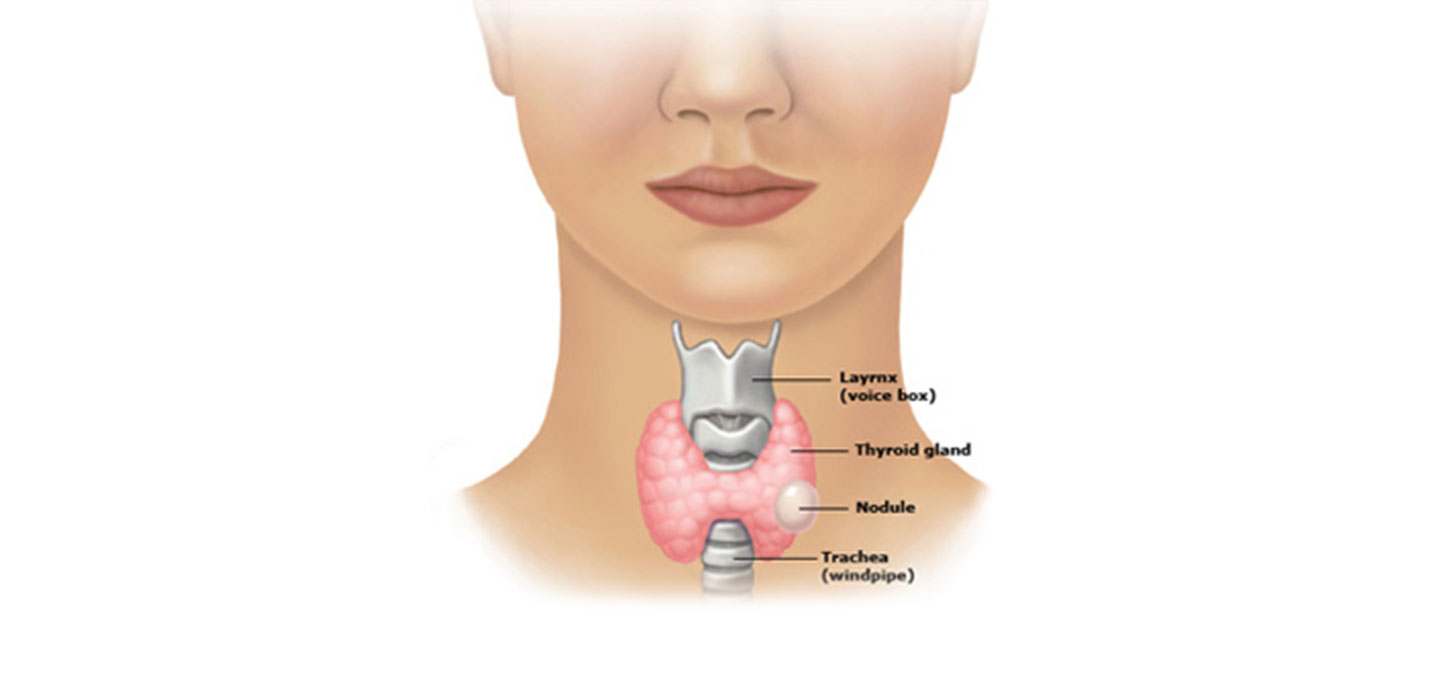
The thyroid is a soft, butterfly shaped gland in the lower central neck that secretes thyroid hormone, essential for the normal function of many organ systems by careful regulation of cell metabolism. A simple analogy is that thyroid hormone is the “gasoline” or “battery” that runs our biological engine at the right pace.
Disease of the thyroid can be broadly classified into two groups:
- problems of hormone production
- problems of nodular disease (growths or lumps within the thyroid gland)
These two problems are usually distinct and independent of one another.
Problems of hormone production (too high or too low) are usually treated with medication.
Problems of nodular disease are managed by a neck ultrasound and an ultrasound-guided fine needle biopsy to determine if surgical management is required.
Neck Ultrasound & Ultrasound-Guided Fine Needle Aspiration Biopsy (FNAB)
An ultrasound is a non-invasive bedside scan that provides very detailed information about the internal appearance and characteristics of the of the thyroid nodule, and a very sensitive and accurate means of distinguishing benign nodules from cancerous ones. The ultrasound is also very useful in evaluating the parathyroid and salivary glands, swollen lymph nodes, neck cysts and other common neck lumps.
Upon detection of a thyroid nodule, the neck step is often to proceed with an ultrasound-guided fine needle aspiration biopsy (FNAB). This is a simple bedside procedure that involves the use of the ultrasound to guide a very fine needle precisely into the nodule, from which a small amount of tissue is taken for histolopathologic diagnosis under the microscope.
The Thyroid Head and Neck Surgery Centre is unique in performing the ultrasound and ultrasound-guided FNAB at the same sitting, with the results of the tissue diagnosis usually made available within the same work day.
Thyroid Nodules
Clinically detectable nodules occur between 4 – 7% of the general population. Small or sublclinical thyroid nodules however, (nodules less than 1 cm that escape detection by clinical examination alone) are exceedingly common, present in about 30% of women under the age of 50 and 50% of women aged above 60.
The most important question to ask when a thyroid nodule is discovered is, what is the likelihood it is benign or cancerous.
The good news for the majority of patients is that 90 – 95% of thyroid nodules are benign.
Indications for Thyroid Surgery include:
- A nodule confirmed to be cancerous on FNAB (Fine Needle Aspiration Biopsy)
- A nodule that is indeterminate or suspicious on the thyroid ultrasound or FNAB
- A nodule that demonstrates progressive growth over time
- A large nodule causing mass effect such as compression of the the windpipe (trachea), gullet (esophagus), or growing down into the chest cavity (a retrosternal goiter)
- A thyroid gland that produces excessive hormone (hyperthyroidism) that has failed medical treatment
Thyroid Surgery
Thyroid surgery is the primary treatment modality for thyroid cancer.
A thyroidectomy, the surgical procedure to remove the thyroid gland, is performed through a curved incision measuring 5 - 8 cm in the lower central neck. It is one of the safest operations performed today, with surgical risks of voice damage or parathyroid dysfunction of less than 1% when surgery is performed by an experienced thyroid surgeon.
It is the most common procedure we perform here at the Thyroid Head & Neck Surgery Centre.
Recovery from thyroid surgery is generally very quick, with most patients being discharged from hospital the day after surgery with normal speech and swallowing, minimal pain or discomfort, and complete independent mobility.
Thyroid Cancer
Thyroid cancer is three times more common in women than in men.
Thyroid cancer is the 5th most common cancer amongst women worldwide and in the United States, is the most common cancer amongst women in South Korea and the 8th most common amongst women in Singapore.
The incidence of thyroid cancer is increasing at about 7% per year globally, faster than any other solid organ cancer.
The reason for this is not known, but this increase spans across thyroid cancers of all sizes, and cannot therefore be attributed to increased diagnostic scrutiny alone.
Alarming as this may sound, three important and encouraging facts should be borne in mind:
- The majority of thyroid cancers are detected while confined to the thyroid gland and at an early stage
- Thyroid cancer is very eminently treatable. Early diagnosis and treatment of thyroid cancers in good risk patients results in cure rates of 98 – 99%, a 20 year prognosis that far surpasses any other solid organ cancer
- Most patients with thyroid cancer return to completely normal lives, livelihoods and physical activity after treatment, without any long-term cosmetic of functional disability
The most significant risk factor for thyroid cancer is a history exposure to ionising radiation. Patients’ age and gender, and nodule size of more than 4 cm are also important considerations.
The most common varieties of thyroid cancer papillary and follicular cancer, collectively referred to as differentiated thyroid cancer, are usually not hereditary or genetically linked.
Management of Thyroid Cancer
Surgery is the main modality of treatment for thyroid cancer. It is required to remove all "gross" or measurable disease. Cure rates are the highest when all cancerous disease is completely and successfully removed.
Radioiodine is often, but not always required after surgery. It is very effective in ablating small cancer cells that cannot be seen on felt, "microscopic" disease, that may lie within the vicinity of the thyroid, in the tissue fluid or in the surrounding lymph nodes. It is typically administered orally 4 - 6 weeks after surgery.
Conventional chemotherapy and radiotherapy are very seldom required for the treatment of thyroid cancer.
- Trusted Singapore Thyroid and Head & Neck Surgeon
- More Than 20 Years’ Experience
- Surgical Expertise in Thyroid Nodules & Cancer
- Personalised Care & Best Practices
- Evidence Based Treatment Options
(Stanford University, USA)
3 Mount Elizabeth #17-07
Mount Elizabeth Medical Centre
Singapore 228510
